At a Glance:
- Diverticulae are pockets that form when the internal layers of the colon bulge out through the outer layer of the colon
- Having one or more diverticulae is referred to as diverticulosis
- When diverticulae become inflamed, damaged or infected, this is referred to a diverticulitis
- Diverticulosis is typically asymptomatic
- Common symptoms of diverticulitis include abdominal pain, bloating, constipation or diarrhea, and in some cases, bloody stool
- Severe or untreated diverticulitis may result in complications including the formation of abscesses, fistula or phlegmon as well as intestinal blockages or perforation and peritonitis
- While an exact cause of diverticulosis is unknown, it is believed that a lack of dietary fibre in the diet may increase the risk of diverticulae forming
- Other risk factors include age, a lack of exercise, obesity, some medications and smoking
- Mild diverticulitis may be treated at home, but severe diverticulitis may require hospitalisation for intravenous antibiotics or even surgery
What is Diverticulitis?
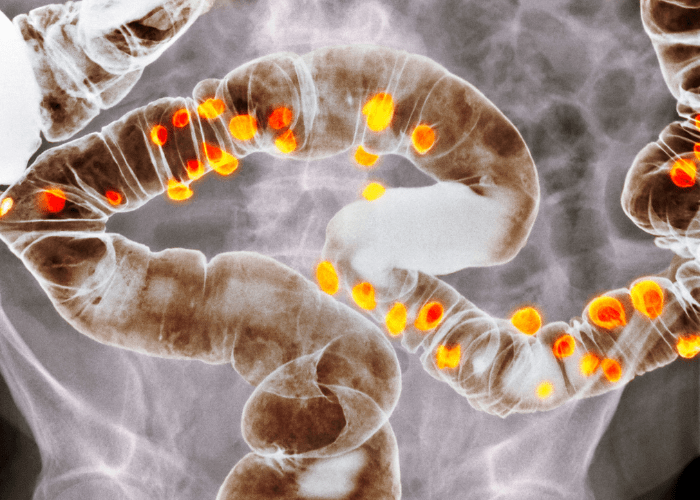
Diverticulae are small sacs that may form and bulge outwards from the lining of the digestive system. These sacs typically form in the lower large intestine (colon), but may form in other parts of the digestive system, including the oesophagus and bladder. These pouches are typically harmless and many people don’t realise they may have them. The presence of one or more diverticulae in the lining of the colon or other part of the digestive tract is referred to as diverticulosis.
Diverticulitis, also known as diverticular disease, occurs when one or more diverticulae become infected and inflamed. The exact reason that diverticulae forms or becomes infected. It is estimated that around 50% of people may have diverticulosis by the age of 50, and around 65% by the age of 80.
Of those people who have developed diverticulosis, the estimates of those that will go on to develop diverticulitis range from as low as 1% to as high as 25%. The symptoms of diverticulitis range from mild to severe and include abdominal pain, bloating, diarrhea, constipation and nausea. In addition to the common symptoms, diverticulitis may lead to a number of potential complications as well.
While age is one of the major contributing factors to the risk of developing diverticulitis, people of any age may develop the condition. It appears as though some people may be born with diverticulae or a propensity to develop diverticulae leading to them appearing in childhood. There also appears to be a correlation between childhood obesity and the early development of diverticulosis.
Studies show that diverticulosis has become more common since the dawn of the 20th century. It is also more common it Western countries, such as Australia, North America and much of Northern Europe, than it is in Asian countries and Africa. This has led to the theory that low fibre diets are a major contributing factor to the development of diverticulosis. This is supported by the fact that it appears that vegetarians are less likely to develop diverticulosis than the general public. In Asian populations the disease appears to be more common on the right side of the large bowel with the reverse being seen in Caucasians.
Symptoms of Diverticulitis
Diverticulosis is typically asymptomatic but some people may experience a number of symptoms, such as abdominal pain and bloating, diarrhoea or constipation, and even rectal bleeding/blood in the stool if the diverticula have formed near a blood vessel.
Diverticulitis is never asymptomatic but the symptoms themselves may vary from mild to severe. Common symptoms include:
- Abdominal Pain - this may be brief and intense or persistent, lasting for days at a time. For some reason that is not yet fully understood, causasians are more likely to develop diverticulae in the lower third of the colon, while Asian people are more likely to develop them in the first third of the colon.
This means that caucasians are more likely to experience the pain centred on the left side of the abdomen whilst Asians are more likely to have the pain centred on the right side of the abdomen - Bloating
- Bloody Stool - diverticulae may bleed due to proximity to blood vessels or due to inflammation and infection
- Constipation or Diarrhea - constipation is more common than diarrhea but both are possible symptoms
- Fever
- Nausea and Vomiting
In addition to the common symptoms of diverticulitis, a number of complications may arise if the condition is left untreated or the infection is severe. Only around 25% of people with diverticulitis develop complications, such as:
- Abscess - an abscess is a pus-filled cavity that may form when a diverticulum becomes infected. These abscesses may burst and spread the infection to surrounding tissues
- Fistula - a fistula is a tunnel of flesh that connects two parts of the body, such as the colon and the abdominal wall. These connections form when two sections of infected tissue touch and become stuck together. Fistulas may cause complications of their own and typically require surgery to correct
- Intestinal Obstruction - scarring caused by an infection may partially or completely block parts of the colon
- Intestinal Perforation - a burst abscess or severely infected diverticulae may lead to a hole in the colon, allowing the contents to spill into the abdominal cavity, leading to infection and inflammation
- Peritonitis - if an infected diverticula bursts, the infection may spread to the lining of the abdomen. Peritonitis is a serious condition and may even be fatal in some cases. Immediate medical attention is required for treatment
- Phlegmon - a phlegmon is an infection that is less contained than an abscess. A phlegmon typically spreads through soft tissue and produces pus
If you experience periods of abdominal pain and bloating, diarrhoea or constipation or have passed bloody stools, there’s no need to panic. While diverticulitis shares a number of symptoms with bowel cancer, it is a far more common condition.
Schedule an appointment to see a doctor to get tests and find out the cause of your pain. The fastest and easiest way to search for and book healthcare appointments online is with MyHealth1st.
What Causes Diverticulitis?
Diverticulae form when pouches of intestinal tissue bulge outwards through the colon. The exact reason for this happening is unknown, but circumstantial evidence appears to show that it may be due to a lack of dietary fibre.
Dietary fibre helps stools remain soft and easily passes. If the diet does not contain enough fibre, the stool becomes hard and requires more pressure in the colon to pass. This additional strain is thought to cause the outer layer of the colon to give way as the inner layer is pushed through it forming a pocket somewhere between the size of a pea and a marble.
Diverticulitis occurs when one or more of these diverticulae become damaged or infected. This may occur when faeces or partially digested food either becomes trapped in a diverticulum or blocks the entrance to a diverticulum.
While the exact cause of diverticulosis is unknown, there are a number of risk factors that may increase the chance of a person developing diverticulae, including:
- Age - the change of someone developing diverticulae increases with age, with an estimated 50% or more of the population having diverticulosis by the time they are 70
- Diet - although this is disputed, a lack of dietary fibre combines with high fat seems to increase the risk of diverticula forming
- Exercise - a lack of physical exercise appears to increase the risk
- Medication - some medications, including steroids, NSAIDS (such as ibuprofen) and opioids are linked to increase instances of diverticulosis
- Obesity - being severely overweight or obese appears to increase risk
- Smoking - smokers are more likely to develop diverticula than non-smokers
Treatment for Diverticulitis
As diverticulosis is commonly asymptomatic there may not be any need for treatment. There is no known way to stop new diverticulae from forming, but in some cases, people with diverticulosis may be advised to change their diet to either add more dietary fibre or avoid certain foods. In some extreme cases, people with a large number of diverticulae may opt to have elective surgery to remove the compromised part of the colon.
Depending on the severity of the diverticulitis, treatment may vary. Mild diverticulitis may be treated at home with antibiotics and a liquid diet until the symptoms subside. Serious diverticulitis requires medical attention and may even require hospitalisation.
Treatments for severe or acute diverticulitis include intravenous antibiotics, drainage of abscesses that may have formed and in some cases, surgery.
Depending on the severity and extent of the damage, there are two major types of surgery performed to treat diverticulitis.
- Primary Bowel Resectioning - during surgery, damaged sections of the bowel are removed and the remaining tissue is reconnected allowing for normal function. Depending on the amount of tissue to be removed, the operation may be performed as open surgery or through minimally invasive laparoscopic means.
- Bowel Resectioning with Colostomy - if the damage and inflammation is severe enough that the remaining colon can’t be reconnected to the rectum, the surgeon will perform a colostomy. During this procedure a stoma (an opening in the abdominal wall) is formed to which the healthy end of the colon is attached. A bag is affixed to the stoma so that waste can be collected and disposed of.
In some cases, the colostomy may be a temporary measure, with the parts of the colon being reconnected and the stoma closed once the inflammation has subsided. In other cases not enough colon remains for resectioning so the colostomy will be permanent.