
“It’s not Lupus!”, was one of the familiar refrains of the very popular and successful medical TV dramedy, House. Thanks to the huge range of symptoms that can accompany Lupus, the autoimmune disease became something of a punchline in the show. Any time someone presented at the hospital with mysterious symptoms, the suggestion that it might be Lupus was thrown out only to be quickly shot down. As amusing as the bit may have been, Lupus really isn’t a joke.
So What is Lupus Anyway?
Lupus is a chronic autoimmune disorder. This means that the body’s immune system attacks its own cells, leading to inflammation. The condition can be localised or systemic, mild or severe, ongoing or intermittent. The varied nature of presentation and the massive number of potential symptoms make Lupus a massively variable disease.
Although lupus is not as common as rheumatoid arthritis or some autoimmune thyroid disorders, it is certainly not a rare condition, typically affecting women more than men.
Most cases are mild, mainly affecting the skin, the joints, the hair and the mouth but in the more severe cases, lupus may be a life-threatening condition if not detected and managed early.
In its most extreme form, lupus may affect the kidneys, the brain, the lungs and the covering of the heart known as the pericardium. There are some subgroups of lupus that can also damage the valves and heart muscle as well.
Depending on where lupus presents and the overall symptoms, the autoimmune disease is broken into four categories:
- Systemic Lupus Erythematosus (SLE) - SLE is the most common form of lupus and is systemic, meaning it can affect the entire body. The severity of SLE can vary from mild to severe, but mild cases are far more common than severe or life threatening. Women of child bearing age and people from Afro-Caribbean or Asian backgrounds are more likely to develop SLE, but anyone can possibly develop the condition. Medical science is yet to pinpoint the exact cause of lupus, but it appears to have both genetic and environmental factors. There is no cure for SLE, but symptoms can be controlled or minimised through medication.
- Discoid Lupus Erythematosus (DLE) – DLE presents on the skin as scaly red patches that mostly appear on skin that is regularly exposed to the sun. Although these lesions most commonly appear on sun-exposed areas, they can also develop on other parts of the body. DLE is a lifelong condition with no cure, but the lesions can be treated with medication and by limiting exposure to sunlight.
- Drug-Induced Lupus – Drug-Induced Lupus isn’t lupus, but rather a number of symptoms that mimic SLE that can be brought on by a reaction to medications. These symptoms will disappear after the medication is stopped.
- Neonatal Lupus – This rare form of lupus is temporary but can affect the skin, heart and blood of a foetus or newborn. Neonatal Lupus is caused when autoantibodies from a mother with SLE are passed to a child before they are born. The condition usually recedes as the child’s own immune system develops.
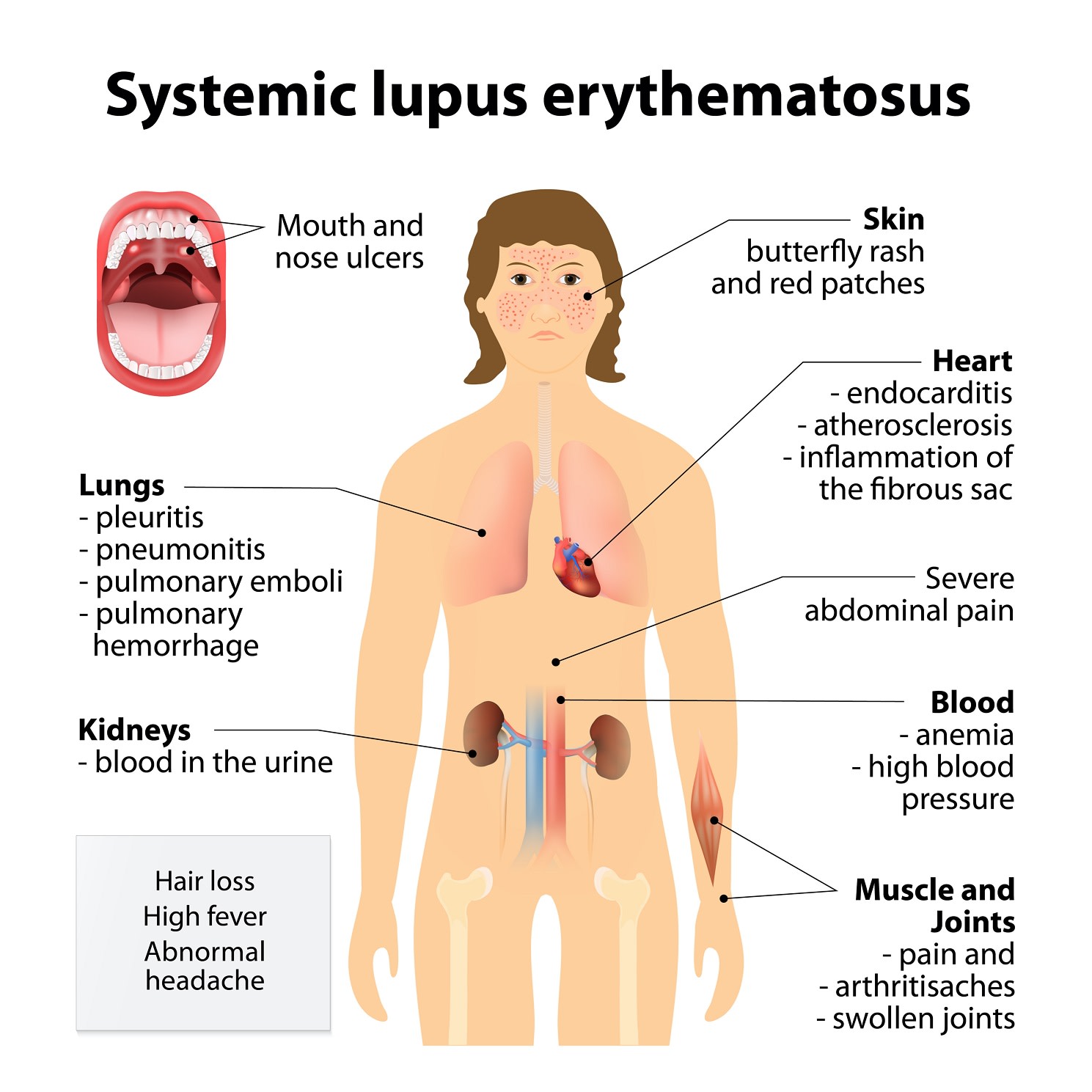
Due to the fact that Lupus can present anywhere in the body, the autoimmune condition has an extremely wide variety of symptoms that can manifest. Discoid Lupus Erythematosus is relatively straightforward to diagnose given the limited set of symptoms, but SLE, usually just referred to as Lupus, can present in a huge number of ways, including:
- Abdominal pain
- Anxiety and depression
- Blood related problems: including anaemia, high blood pressure/hypertension and increased risk clotting
- Chest pain
- Cognition, confusion and memory issues
- Fatigue
- Fever
- Hair loss
- Headaches or migraines
- Muscle and joint pain
- Rashes: face and body
- Reduced kidney function
- Seizures
- Shortness of breath
- Ulcers: nose and mouth
- Visual disturbances
These symptoms are caused by inflammation in an associated area - chest pain and shortness of breath for example are caused by inflammation in the tissues surrounding the heart or lungs - but vary markedly in severity. It’s unlikely that a person with lupus will experience all of the symptoms, but may experience a number. While some people with lupus have relatively stable symptoms, the flare-ups may be unpredictable and become more severe. Triggers for flares vary from person to person but high stress and exposure to UV radiation are common triggers.
Depending on the severity, nature and presentation of symptoms, lupus can be very difficult to diagnose. The blood test for lupus is known as anti-nuclear factor. It is certainly not definitive but a negative test makes the diagnosis unlikely.
Diagnosis may take time but it is important. Having lupus diagnosed early means that it can be treated and controlled, rather than letting the symptoms and damage become more serious with time.
If you’re experiencing a number of strange symptoms and Dr House isn’t around to diagnose you, the easiest and fastest way to find and book a doctor’s appointment is with MyHealth1st.
Treatments for and Living With Lupus
There is no cure for lupus, but individual symptoms can be controlled through the use of medications. Pain relievers, corticosteroids, non-steroidal anti-inflammatory drugs and even hydroxychloroquine are used to mitigate different symptoms. In moderate to severe cases of lulus, immunosuppressants - drugs that suppress an overactive immune system - may be used.
In addition to medications, there are a number of lifestyle and self-care strategies that people can adopt to help control lupus, including:
- Avoid or mitigate exposure to UV light – sunlight is a common trigger for flares, especially in skin rashes, but in some cases the UV from fluorescent light can act as a trigger as well. Keeping covered, wearing a hat and using 50+ UVA sunscreen can help limit exposure to UV rays.
- Exercise regularly – aside from the fact that regular exercise has general health benefits, it can also help you manage symptoms of lupus, reduce stress (a common trigger for flares) and manage pain. Regular exercise can increase energy levels to counteract fatigue, can help better regulate sleep cycles, increasing energy and cognition while lowering stress and can strengthen the body to help fight muscle and joint pain. Keeping fit can also help stave off potential long term effects of lulus including heart disease and osteoporosis.
- Maintain balance – balancing work and rest can help maintain energy levels and cope with fatigue. Maintaining a healthy work/life balance can also help in reducing stress and lessening the frequency of flare ups.
- Manage your stress – stress is a major trigger for flares, so learning ways to mitigate or deal with stress is a valuable way of limiting symptoms. Not everyone deals with stress the same way, so finding a technique that works for you, whether it’s meditation, yoga, going for a walk, having a long hot bath, listening to music or the like is an important self-care technique.
- Quit smoking – Smoking can increase the severity of some lupus symptoms and can reduce the effectiveness of some medications.
- Understand your symptoms – by carefully monitoring your symptoms you can pinpoint the triggers for flares and (hopefully) avoid them.
As with most conditions, the key to management is early detection, Along with appropriate pharmaceutical therapy. If you are diagnosed with lupus, it is vital you have a long-term relationship with a trusted specialist in the area. Typically this is a rheumatologist or immunologist.
Musculoskeletal Australia hosts a network of support groups for people living with musculoskeletal conditions, including Lupus, in Australia. Support groups offer people living with a condition the chance to talk to other people with the same condition, to share stories, tips of self-care and offer emotional support as someone who knows your struggles.